Is Unpredictable Menstruation Complicating your Life, Impacting your Daily Activities, and Making it Difficult for you to Plan Ahead?
 Do you find your periods come at irregular intervals? Maybe you’ve noticed that your menstrual flow and other period symptoms vary widely from month to month. You may be experiencing irregular menstruation, known by the medical term as oligomenorrhea. This is a very common symptom of PCOS, and women report that it directly impacts their quality of life.
Do you find your periods come at irregular intervals? Maybe you’ve noticed that your menstrual flow and other period symptoms vary widely from month to month. You may be experiencing irregular menstruation, known by the medical term as oligomenorrhea. This is a very common symptom of PCOS, and women report that it directly impacts their quality of life.
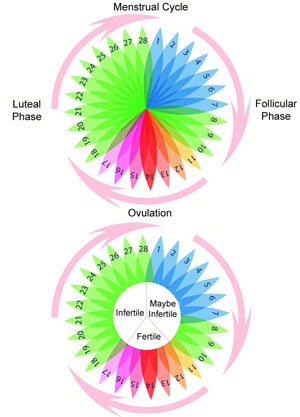
What is oligomenorrhea? It is characterized by infrequent, unpredictable menstruation. Your cycles can be widely and irregularly spaced. Your periods can range from very light to very heavy. They might or might not be accompanied by excessive pain, cramping, bloating, and discomfort. Irregular menstruation is also a classic symptom of PCOS.2 Often accompanying infrequent menstruation is irregular cycles and menstrual flows. For example, women with PCOS can fail to menstruate for a few months and then experience an extremely heavy period, followed by spotting later in the same month.
Nine or fewer menstrual cycles per year is a common diagnostic criterion for PCOS. In fact, women often discover they have PCOS by seeking help for infrequent or irregular periods. What is very worrisome is that irregular menstruation can be a warning sign of future infertility problems. Even if you aren’t trying to conceive now, you might be worried about your ability to become pregnant in the future.
If you’ve struggled with irregular menstruation for years due to PCOS, there is plenty of reason for hope! What can you do if you have been experiencing infrequent or irregular menstruation associated with PCOS? If you have time, read the in-depth information in below to learn more about the causes of menstrual irregularity and your treatment and supplementation options. We know you’re busy! If you’re ready to proceed on your journey back to good health, contact us. Our dedicated team is committed to restoring the health of women with PCOS. Insulite Health wants to be your partner in your quest for good health.
+ Click here to learn about the all natural PCOS 5-Element Solution
+ Click here to read more articles about PCOS and Menstrual Irregularities
Causes
Amenorrhea is a Common Symptom of
Polycystic Ovarian Syndrome
Irregular and infrequent periods are a common, and bothersome, symptom of PCOS. What explains the wide variations in periods that women with PCOS face far too often?
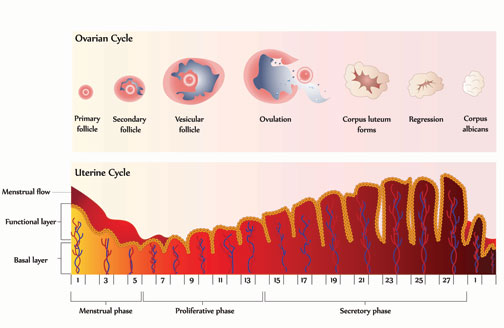
First, a preliminary discussion of ‘normal’ menstruation. Your periods are controlled by a complex interplay of multiple hormones. Some hormones play a greater role at the beginning of the menstrual cycle, whereas others play a greater role at the conclusion of the cycle. Each month, hormones trigger one of the ovaries to release an egg for possible fertilization. The egg travels from the ovary toward the uterus via the fallopian tubes. Meanwhile, more hormones prepare the uterus for possible pregnancy. This includes building up the lining of the uterus. If the egg isn’t fertilized before it reaches the uterus, the uterine lining sheds, and a menstrual period begins.5
In PCOS this normal menstrual process is disrupted by improper hormone levels. As explained by womenshealth.gov: “The ovaries … have tiny fluid-filled sacs called follicles or cysts. As the egg grows, the follicle builds up fluid. When the egg matures, the follicle breaks open, the egg is released, and the egg travels through the fallopian tube to the uterus … In women with PCOS, the ovary doesn’t make all of the hormones it needs for an egg to fully mature. The follicles may start to grow and build up fluid but ovulation does not occur. Instead, some follicles remain as cysts. For these reasons, ovulation does not occur and the hormone progesterone is not made. Without progesterone, a woman’s menstrual cycle is irregular or absent. Plus, the ovaries make too many male hormones, which also prevent ovulation.”
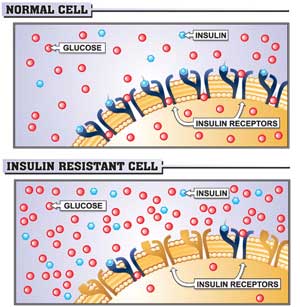
We know PCOS is characterized by imbalances in male and female sex hormones, but what causes that imbalance in the first place? The likely answer is Insulin Resistance, also called IR. Insulin is a powerful hormone and is responsible for regulating metabolism, a critical bodily function. If your cells do not respond properly to insulin, the condition of Insulin Resistance can develop. In response, your body increases its production of insulin and chronically high levels of insulin can take a toll on many bodily systems and organs. PCOS is the disorder that results when high insulin levels harm the endocrine system and the ovaries. The key to improving your health is recognizing this underlying cause of PCOS, Insulin Resistance, and taking action to manage this condition and improve your overall health and wellbeing.
Symptoms
Have you been Experiencing Fluctuations in your Menstrual Cycles?
 Perhaps you’ve gone for years without having normal monthly periods? Women with PCOS often must endure infrequent or irregular menstrual cycles and experience a number of interrelated symptoms pertaining to menstrual irregularity. Struggling with the unpredictability of your menstruation isn’t fun, but gaining knowledge about your symptoms can be the first step in finding relief.
Perhaps you’ve gone for years without having normal monthly periods? Women with PCOS often must endure infrequent or irregular menstrual cycles and experience a number of interrelated symptoms pertaining to menstrual irregularity. Struggling with the unpredictability of your menstruation isn’t fun, but gaining knowledge about your symptoms can be the first step in finding relief.
If you’re having fewer than nine menstrual cycles per year (and are not pregnant), there is a good chance you are failing to ovulate, known as anovulation, at least some of the time. Anovulation can result in missed periods, but menstrual periods can still occur even when ovulation has failed. These cycles are known as anovulatory cycles. Anovulatory cycles are characterized by a very light flow with short duration and usually lack other normal menstrual symptoms, such as breast tenderness.1
In other cases, women with PCOS still ovulate, but do so infrequently. If menstrual periods are spaced more than 35 days apart, this is known as oligomenorrhea, or infrequent menstruation. Delayed ovulation can result in an overgrowth of the endometrial lining of the uterus and can cause an unusually heavy menstrual flow. This might or might not be accompanied by dysmenorrhea (excessive menstrual pain). This pain can even be severe enough to require treatment with prescription pain medications.2
Want to learn more about painful, prolonged menstruation and PCOS?
Whether you are having an unusually light flow or an unusually heavy flow, both are likely indications of hormonal disruption to your menstrual cycle. Women with PCOS typically have high levels of androgens (male sex hormones). In addition to infrequent periods, irregularly spaced periods, and irregular menstrual flows, women with PCOS can also experience complete amenorrhea (absence of menstruation), heavy/prolonged periods, and extreme menstrual cramps and pain. Women can develop symptoms at a young age. In fact, adolescents as young as 12 have been diagnosed with PCOS. Many women diagnosed with PCOS report their difficult periods began in their teens.
Complications

Coping with irregular periods? Unpredictable cycles, heavy menstrual flows, and excruciating pain make it hard for women to engage in life and can make them feel trapped by their own bodies. But the frustrating symptoms aren’t the end of the story. Menstrual irregularity related to PCOS is a frequent precursor to infertility problems. Left untreated, women can later face problems when they’re ready to conceive, or have other problems during pregnancy, such as greater rates of miscarriage and stillbirth.
Learn more about pregnancy problems and PCOS
Also, PCOS is associated with a higher risk of other serious illnesses, including: high cholesterol, high blood pressure, cardiovascular disease, metabolic syndrome (syndrome X), reproductive system cancers, liver disease, and diabetes. Please take time to educate yourself about these potential PCOS complications and learn what you can do to protect yourself. If you think you could be at risk of developing or if you have already noticed symptoms of these illnesses, talk to your health-care provider at once.
Natural Therapies
What Can be Done for Menstrual Irregularities?

There are various nutritional supplements that can be helpful in managing the menstrual symptoms stemming from PCOS. Vitex Agnus Castus, commonly known as Chaste Tree Berry, has been used by European women for menstrual problems for centuries. Chaste Tree Berry can improve menstrual regularity by normalizing levels of the hormones associated with the luteal phase (or last half) of the menstrual cycle. Chaste Tree Berry is especially helpful to women with PCOS since it also can respond to hyperprolactinemia (high levels of prolactin), a suspected culprit in many PCOS symptoms.
 Another useful botanical remedy for PCOS is Urtica Dioica, or Stinging Nettle. The root of the Stinging Nettle plant helps the body maintain healthy levels of sex hormones by increasing SHBG (sex hormone-binding globulin). SHBG is not a hormone itself, but affects the bioavailability of sex hormones in the bloodstream. SHBG levels are often low in women with PCOS, and can be a factor in the intensity of PCOS symptoms, especially symptoms relating to the imbalance of sex hormones, like menstrual problems.
Another useful botanical remedy for PCOS is Urtica Dioica, or Stinging Nettle. The root of the Stinging Nettle plant helps the body maintain healthy levels of sex hormones by increasing SHBG (sex hormone-binding globulin). SHBG is not a hormone itself, but affects the bioavailability of sex hormones in the bloodstream. SHBG levels are often low in women with PCOS, and can be a factor in the intensity of PCOS symptoms, especially symptoms relating to the imbalance of sex hormones, like menstrual problems.
Flaxseed is another commonly used plant-based remedy for PCOS. Flaxseed supports the metabolism of estrogen. This has a beneficial effect on the production of protective estrogen metabolites and helps the body increase SHBG (sex hormone-binding globulin) levels, which can be chronically low in women with PCOS.
Finally, PCOS sufferers should consider adding Saw Palmetto to their supplementation regimen. The berries of the Saw Palmetto plant contain a natural 5-alpha reductase inhibitor, which can impede testosterone conversion, helping the body to stabilize the levels of male sex hormones (androgens).
Dietary Changes and Exercise

The primary PCOS treatment recommended by doctors is a healthy lifestyle. Lifestyle modifications such as eating a lower-calorie diet, losing weight, and becoming more physically active can minimize many issues involved with PCOS. The changes in your body and your health can be nothing short of miraculous! Ovulation can be restored, pregnancy rates improved, and blood pressure and androgen levels lowered — without medication or surgery or other means.7
Choose the very best foods for your PCOS diet! You deserve the best nutrition and best quality foods to restore your health. Limit processed foods and added sugars and add more fruits, vegetables, lean meats, and whole-grains. Doing so will lower blood glucose (sugar) levels, improve the body’s use of insulin, and normalize hormone levels in your body. Even just losing 10 percent of your body weight can have positive effects such as restoration of normal menstrual cycles.3
In addition to improving diet and exercise, the Insulite PCOS System goes a step further by supporting women struggling with difficult food cravings. A core element of our system is an awareness of the addictive power of food and the biology of thought that underpins it. Insulite’s nutritional supplements are designed to help correct the underlying body chemistry imbalances that trigger food cravings. Another core element of the Insulite PCOS System is that Insulite Health provides direct support to women struggling with PCOS by providing free consultations with our skilled team, weekly health tips by email, and by connecting you with other women suffering from this condition online.
Treatment Options
Which Option is Best for You?
Treatment options for menstrual irregularities in PCOS include birth control, insulin sensitizers, and lifestyle changes.

Birth Control Pills
Birth control pills, or oral contraceptives, are a common treatment for women with PCOS menstrual symptoms who also want to avoid pregnancy. The combination of hormones in birth control pills regulates ovulation and periods and reduces hirsutism and acne by lowering androgen production. There isn’t a single birth control pill that’s better than another for treating PCOS, but if you do have hirsutism or acne, an oral contraceptive without androgenic properties is probably better for you.7 Birth control pills can also help with premenstrual syndrome (PMS), heavy menstrual flow, anemia related to menstrual bleeding, and reducing your chances of developing endometrial cancer, ovarian cancer, and ovarian cysts.4 Many women report less severe cramps when taking oral contraceptives.3
Insulin Sensitizers
Insulin, a hormone that controls the conversion of sugar, starches, and other food into energy to store or use, is also linked to PCOS. Women who have PCOS symptoms often have an excess of insulin, which increases the production of androgens (male hormones). These hormones lead to acne, excessive hair growth, weight gain, and ovulation problems.3 Insulin-sensitizing agents “make the body more sensitive to the available insulin” and they can regulate periods and ovulation, as well as reduce infertility, minimize hirsutism, and reduce acne.7
One of the most commonly prescribed insulin sensitizers is Metformin, also known as Glucophage. Although not originally intended for PCOS (Metformin is a drug for Type-2 Diabetes), it is effective in women with PCOS because PCOS and diabetes can have the same underlying cause, Insulin Resistance. Metformin has a favorable track record but it is not without risks. Check the Side Effects tab to learn more about your risks.
What Are the Side Effects you Might Experience?

If you’re considering pharmaceutical treatment of your menstrual irregularities due to PCOS, you might have questions and concerns about the possible side effects of these medications. Below is a summary of the most common side effects of birth control pills, or oral contraceptives, and Metformin, a common insulin-sensitizing medication. Never hesitate to ask your doctor about any side effect you may be experiencing! Some side effects can be serious and should be treated at once.
Birth Control Pills
The side effects of birth control pills include spotting, nausea, headaches, mood changes, breakouts, sore or enlarged breasts, and weight changes. However, these side effects are usually manageable.4
Spotting, or very light bleeding, normally happens in the first three weeks as your body adjusts to the pill. It is not serious, although if it becomes heavy for longer than a few days, contact your health-care provider. Nausea can be cured when the pill is taken with food, headaches and mood changes are often related to other factors, and acne breakouts can happen to some women when they take a certain kind of birth control pill. Sore or enlarged breasts are also a possibility, but the tenderness should go away on its own. Weight gain and weight loss are also possible side effects; however, most women stay the same weight. According to youngwomenshealth.org, most women think they gain 5-10 pounds, but there is no change in their weight once checked by a health-care provider.
Some side effects of oral contraceptives can be serious. If you develop severe abdominal or stomach pain, chest pain, leg pain in the calf or thigh, vision or speech problems, dizziness, weakness, numbness, shortness of breath, or a severe cough, get medical assistance immediately. Always speak to your health-care provider regarding any questions you have about how to take your prescription medications or how to treat side effects. Side effects often go away in the first three or four months. If they persist beyond that or are too uncomfortable to tolerate, then your health-care provider might need to alter your prescription. 
Insulin Sensitizers
One of the most common insulin-sensitizing medications is Metformin, also known as Glucophage. Metformin is an oral medication originally approved for use in treating diabetes.
Some of the most common Metformin side effects are:
- Allergic reaction – itching, rash, wheezing, hives.
- Changes in taste
- Muscle pain
- Diarrhea, abdominal pain, bloating
- Difficulty breathing
- Dizziness
- Electrolyte disturbance
- Excessive thirst
- Flu-like symptoms-muscle pain, fever, chills, and weakness
- Flushing or reddening of the skin, commonly on the face
- Forcefully beating heart (heart palpitations)
- Interference with vitamin B-12 absorption
- Kidney problems
- Liver problems
- Nail problems
- Sweating
- Thyroid hormone disruption
This is quite a range of side effects and these are only the most common. If you are taking an insulin sensitizer, report all of your side effects to your doctor, including any not mentioned here. Additionally, most doctors recommend immediately ceasing use if you become pregnant. Although Metformin hasn’t been shown to cause birth defects, it is generally discouraged.
Next Steps
- Take the PCOS Quiz! Get your score and assess your hormone health risks.
- Join our Facebook Sisterhood Group Pose your questions to this group of like-minded women. Get the answers to your questions and the support you need.
- Checkout the Hormone Reset. Guided Practices to eliminate anxiety, lose weight and boost energy.
We are committed to helping women reverse their symptoms of hormone imbalance – a major cause of excess weight gain, adult acne, unwanted facial hair, depression, anxiety, and heartbreaking female infertility.
©Insulite Health empowers women with hormone imbalance to transform their lives through a process of healing with the Natural Hormone Solution –a complete solution for helping women reverse the symptoms hormone imbalance..

