Are Women with PCOS at Greater Risk for Low Birth Weight?
 “Small gestational age” refers to babies who weigh below the 10th percentile for their gestational age. This is distinct from a premature birth. Babies carried to full term, but weighing below 2,500 grams (5 lbs., 8 oz.) are considered to have a low birth weight. Today, women with PCOS (Polycystic Ovarian Syndrome) can be at twice the risk of a low birth weight baby, and should strive to be as healthy as possible during pregnancy to avoid this outcome. A successful PCOS Pregnancy is possible when you engage in a healthy diet, regular exercise, and pharmaceutical and/or nutritional supplementation, along with good prenatal care.
“Small gestational age” refers to babies who weigh below the 10th percentile for their gestational age. This is distinct from a premature birth. Babies carried to full term, but weighing below 2,500 grams (5 lbs., 8 oz.) are considered to have a low birth weight. Today, women with PCOS (Polycystic Ovarian Syndrome) can be at twice the risk of a low birth weight baby, and should strive to be as healthy as possible during pregnancy to avoid this outcome. A successful PCOS Pregnancy is possible when you engage in a healthy diet, regular exercise, and pharmaceutical and/or nutritional supplementation, along with good prenatal care.
+ Click here to learn about the all natural PCOS 5-Element Solution
+ Click here to read more articles about PCOS and Pregnancy
Health Risks
Pregnancy Problems beyond Low Birth Weight
Many of the pregnancy problems women with PCOS face are similar to those common in women with diabetes, probably because of the higher occurrence of diabetes in women with PCOS. Some of these risks include the following:

- Miscarriage or early pregnancy loss – The exact reason women with PCOS are at higher risk for miscarriage is uncertain. Obesity is an independent risk factor for miscarriage, so it’s not clear whether it’s the PCOS or the obesity that contributes to miscarriage. Because many women who are obese are also insulin resistant, researchers are exploring whether or not reducing Insulin Resistance can improve pregnancy outcomes. NICHD-supported research has shown that treatment with the insulin-sensitizing drug Metformin can significantly reduce the risk of miscarriage in pregnant women with PCOS.
- Gestational diabetes – This condition is a type of diabetes that only pregnant women get. Pregnancy is usually associated with some degree of Insulin Resistance, but the body can usually make up for it and function normally. In gestational diabetes, the body can’t make up for the Insulin Resistance, and the woman gets diabetes while she is pregnant. If controlled, gestational diabetes does not usually result in immediate problems for the mother or the fetus. In most cases, the diabetes goes away after the baby is born. Women who have had gestational diabetes and their children are at higher lifetime risk for type 2 diabetes.
 Preeclampsia – This syndrome is marked by a sudden increase in blood pressure after the 20th week of pregnancy. Preeclampsia can affect the mother’s kidney, liver, and brain. If left untreated, the condition can be fatal for the mother or the fetus. Preeclampsia can lead to eclampsia, a more severe form that can cause seizures and coma in the mother. Daily or weekly blood pressure checks are useful in detecting sudden changes in blood pressure.2 Currently, the only cure for preeclampsia is delivering the fetus. When a woman gets preeclampsia the health-care provider will try to develop a plan to prolong the pregnancy to give the fetus more time to grow and mature. This plan can include giving the mother medications to help prevent seizures and maintain blood pressure levels within a normal range. At the same time, the health-care provider will closely watch the health of the mother for signs that the fetus needs to be delivered right away, even prematurely if necessary.
Preeclampsia – This syndrome is marked by a sudden increase in blood pressure after the 20th week of pregnancy. Preeclampsia can affect the mother’s kidney, liver, and brain. If left untreated, the condition can be fatal for the mother or the fetus. Preeclampsia can lead to eclampsia, a more severe form that can cause seizures and coma in the mother. Daily or weekly blood pressure checks are useful in detecting sudden changes in blood pressure.2 Currently, the only cure for preeclampsia is delivering the fetus. When a woman gets preeclampsia the health-care provider will try to develop a plan to prolong the pregnancy to give the fetus more time to grow and mature. This plan can include giving the mother medications to help prevent seizures and maintain blood pressure levels within a normal range. At the same time, the health-care provider will closely watch the health of the mother for signs that the fetus needs to be delivered right away, even prematurely if necessary.
- Pregnancy-induced high blood pressure – Unlike preeclampsia, pregnancy-induced high blood pressure is a general increase in blood pressure that can begin before the 20th week of pregnancy. If not treated, the condition could lead to preeclampsia. Having high blood pressure can impact delivery of the baby, in that surgical delivery (Cesarean delivery) might be safer for both mother and baby.3
- Preterm birth – Preterm birth is defined as delivery before 37 weeks of gestation. Many researchers believe the higher risk of preterm birth is the result of more pregnant women with PCOS having preeclampsia. Preterm infants are at risk for a number of health problems, including low birth weight and under-developed lungs.
- Cesarean delivery – This surgical delivery is more common among women with PCOS because they are more likely to deliver preterm, they are more likely to be obese (sometimes a reason for this type of delivery), and they are more likely to have pregnancy-induced high blood pressure. Because it is a surgical procedure, recovery from Cesarean delivery can take longer than recovery from vaginal birth.1
Symptoms
Polycystic Ovarian Syndrome as a Multi-Organ Condition

The manifestations of PCOS are diverse and up to 50 percent of patients are normal weight. In many cases, however, the severity of symptoms can be related to abdominal obesity. Abdominal obesity and increased activation of the in?ammatory system is seen in both normal weight and obese patients with PCOS, leading to an increased risk of dyslipidemia, diabetes, and possibly cardiovascular disease. Increased in?ammation in PCOS can be measured as decreased adiponectin levels and increased levels of adipokines, chemokine, and interleukins.1
Abdominal obesity and Insulin Resistance stimulate ovarian and adrenal androgen production, whereas SHBG (sex hormone-binding globulin) levels are decreased. Increased testosterone levels can further increase abdominal obesity and in?ammation. Therefore, PCOS is a vicious cycle, which can be broken by lifestyle modi?cation, insulin sensitizers such as Metformin, or inhibition of testosterone levels.
PCOS can be the result of genetic alterations leading to increased androgen levels in utero, resulting in a predisposition to develop early puberty and later on PCOS. Because of the high prevalence of PCOS and the long-term implications on metabolic risk factors, fertility, and quality of life, general practitioners need to be aware of the syndrome in daily practice. However, there might be a natural solution for you.
Causes
Body Composition and Fat Metabolism in Polycystic Ovarian Syndrome

Approximately 75 percent of patients with PCOS are overweight, but a high waist-to-hip ratio (WHR) indicating increased abdominal fat mass is seen in both normal and overweight patients with PCOS. Increased fat ingestion in patients with PCOS vs. controls was found in some studies, but could not be reproduced by others. Ghrelin and cholecystokinin secretion following meals are impaired in PCOS, suggesting changed appetite regulation. In a recent article, the prevalence of eating disorders was 36.3 percent in women presenting with hirsutism, and conversely, PCOS was over-represented in bulimic women. These results suggest that eating disorders are prevalent in PCOS.
The metabolic rate is not decreased in patients with PCOS, and randomized studies show no differences in the ability to loose weight between patients with PCOS and weight-matched controls on the same diet. In previous studies, decreased quality of life in PCOS was associated with increased body weight and when using SF-36, patients with PCOS had similar scores as patients with chronic diseases such as diabetes and asthma.2
Increased intra-abdominal fat is of central importance in PCOS because it affects growth hormone (GH) secretion, Insulin Resistance, lipid metabolism, and inflammatory status. Lifestyle modi?cation and weight loss improves ovulation rate and fertility and testosterone levels are decreased. In a recent position statement from the Androgen Excess Society, the current evidence for lifestyle intervention and dietary treatment in PCOS is reviewed. It is generally accepted that a more than 5 – 10 percent weight loss improves fertility and menstrual cycles in women with PCOS. To date, there is insufficient evidence to recommend a specific diet in PCOS. Some diet types are more beneficial on metabolic status, but the drop out rate in previous studies was high and the patient’s individual preferences are important to maintain lifestyle intervention and weight loss.
Metformin treatment alone is not followed by weight loss, but can improve the weight loss when combined with lifestyle intervention. A few studies have examined the effect of gastric bypass and gastric banding in PCOS, and found significant improved metabolic risk pro?le, hirsutism, and menstrual cycles after surgery.
 Adrenal hyperactivity in Polycystic Ovarian Syndrome
Adrenal hyperactivity in Polycystic Ovarian Syndrome
Ovarian suppression with long-acting GnRH-agonist leads to higher androgen levels in patients with PCOS than controls. Dehydroepiandrosterone-sulphate (DHEAS) is mainly produced in the adrenal glands and therefore increased DHEAS levels can be used as a marker of increased adrenal activity in PCOS. DHEAS levels decrease with age in PCOS and in controls. Brothers of patients with PCOS have increased DHEAS levels suggesting that adrenal hyperactivity may be an inherited trait of PCOS.
About 25 – 50 percent of patients with PCOS have increased ACTH-stimulated 17OHP responses, which may be caused by CYP21 defects or a more general adrenal hyperactivity (Figure 1). CYP21 defects are autosomal recessive disorders, causing decreased cortisol secretion by the adrenals due to decreased activity of the 21-hydroxylase enzyme. Initial studies reported that more than 20 percent of hyper-androgen patients were CYP21 carriers compared to a prevalence of less than 5 – 10 percent in the background population.
Increased hypothalamic-pituitary-adrenal (HPA) activity in PCOS may be caused by hyperinsulinemia. Insulin stimulates the serine phosphorylation of P450c17 causing increased lyase activity and thereby increased conversion of 17OH pregnenolone to DHEAS in the adrenal glands. Cross-sectional studies in PCOS populations, however, found no signi?cant correlations between DHEAS and fasting insulin. The results of studies using insulin-sensitizing treatment have been con?icting as some studies reported unchanged adrenal androgen levels, whereas other studies found decreased adrenal activity during Metformin or PPARg agonist treatment.
Previous studies reported increased urinary excretion of cortisol metabolites in patients with PCOS compared to controls, which may cause compensatory hyperactivity of the HPA-axis. Increased hepatic 5a-reductase activity was ?rst suggested as a mechanism for increased cortisol metabolism in PCOS and later supported by other studies. 5a-reductase activity correlated with Insulin Resistance in PCOS and insulin sensitizing treatment was followed by decreased 5a-reductase activity in animal studies and in PCOS.1
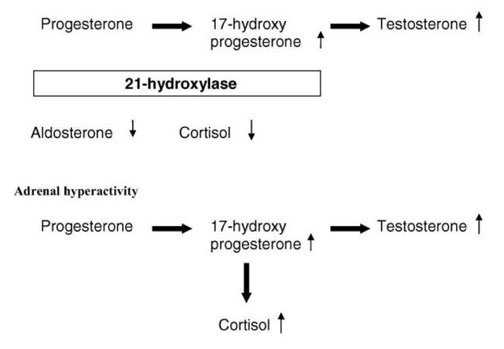
Figure 1. Mechanisms for increased 17-hydroxyprogesterone levels in PCOS. In CYP21 defects, cortisol levels are relatively decreased in contrast to adrenal hyperactivity. As discussed above, increased 17-hydroxyprogesterone levels in PCOS are most often caused by increased adrenal activity. The mechanism for adrenal hyperactivity might be a hypersensitive HPA axis and/or increased cortisol turnover due to increased 5a-reductase activity.
Getting Control of Your PCOS Today
 The primary influence of PCOS is Insulin Resistance – your body’s natural ability to manage ‘blood sugar’ correctly. The good news is you can control Insulin Resistance, and as a result PCOS, to increase your chances of having a healthy baby. It starts with a healthy diet of fruits, vegetable, lean proteins, and complex carbohydrates low on the glycemic scale. As for what to avoid, steer clear of processed foods, sugar products, and simple carbohydrates (such as white bread and pasta). There are also targeted Nutritional Supplements (vitamins, minerals, and botanicals) you can take to win the battle with PCOS. The final component is exercise and staying fit. It’s not always easy to change life habits or to find the materials you need to make smarter eating / lifestyle choices. That’s where Insulite Health can help you. Here, with the Insulite PCOS System, you’ll find information about PCOS and a nutritional / exercise program that allows you to manage PCOS so you, and your baby, can have a happy, healthy life.
The primary influence of PCOS is Insulin Resistance – your body’s natural ability to manage ‘blood sugar’ correctly. The good news is you can control Insulin Resistance, and as a result PCOS, to increase your chances of having a healthy baby. It starts with a healthy diet of fruits, vegetable, lean proteins, and complex carbohydrates low on the glycemic scale. As for what to avoid, steer clear of processed foods, sugar products, and simple carbohydrates (such as white bread and pasta). There are also targeted Nutritional Supplements (vitamins, minerals, and botanicals) you can take to win the battle with PCOS. The final component is exercise and staying fit. It’s not always easy to change life habits or to find the materials you need to make smarter eating / lifestyle choices. That’s where Insulite Health can help you. Here, with the Insulite PCOS System, you’ll find information about PCOS and a nutritional / exercise program that allows you to manage PCOS so you, and your baby, can have a happy, healthy life.
Next Steps
- Take the PCOS Quiz! Get your score and assess your hormone health risks.
- Join our Facebook Sisterhood Group Pose your questions to this group of like-minded women. Get the answers to your questions and the support you need.
- Checkout the Hormone Reset. Guided Practices to eliminate anxiety, lose weight and boost energy.
We are committed to helping women reverse their symptoms of hormone imbalance – a major cause of excess weight gain, adult acne, unwanted facial hair, depression, anxiety, and heartbreaking female infertility.
©Insulite Health empowers women with hormone imbalance to transform their lives through a process of healing with the Natural Hormone Solution –a complete solution for helping women reverse the symptoms hormone imbalance..


 Preeclampsia – This syndrome is marked by a sudden increase in blood pressure after the 20th week of pregnancy. Preeclampsia can affect the mother’s kidney, liver, and brain. If left untreated, the condition can be fatal for the mother or the fetus. Preeclampsia can lead to eclampsia, a more severe form that can cause seizures and coma in the mother. Daily or weekly blood pressure checks are useful in detecting sudden changes in blood pressure.2 Currently, the only cure for preeclampsia is delivering the fetus. When a woman gets preeclampsia the health-care provider will try to develop a plan to prolong the pregnancy to give the fetus more time to grow and mature. This plan can include giving the mother medications to help prevent seizures and maintain blood pressure levels within a normal range. At the same time, the health-care provider will closely watch the health of the mother for signs that the fetus needs to be delivered right away, even prematurely if necessary.
Preeclampsia – This syndrome is marked by a sudden increase in blood pressure after the 20th week of pregnancy. Preeclampsia can affect the mother’s kidney, liver, and brain. If left untreated, the condition can be fatal for the mother or the fetus. Preeclampsia can lead to eclampsia, a more severe form that can cause seizures and coma in the mother. Daily or weekly blood pressure checks are useful in detecting sudden changes in blood pressure.2 Currently, the only cure for preeclampsia is delivering the fetus. When a woman gets preeclampsia the health-care provider will try to develop a plan to prolong the pregnancy to give the fetus more time to grow and mature. This plan can include giving the mother medications to help prevent seizures and maintain blood pressure levels within a normal range. At the same time, the health-care provider will closely watch the health of the mother for signs that the fetus needs to be delivered right away, even prematurely if necessary.